HIPAA Annual Risk Analysis and Management Plans: Leveraging FAIR for Quantitative Risk Management
Introduction: The Evolving Landscape of Healthcare Risk Management
Healthcare organizations face a constant barrage of information security challenges, from stringent regulatory compliance and devastating data breaches to the ever-evolving landscape of cyber threats. While the industry isn't lacking in frameworks and control libraries, effectively implementing them often feels like an uphill battle. We have the tools, but we're struggling to use them strategically.
 FAIR Institute member Darren Shady is an independent contractor and professional educator specializing cyber risk & FAIR’s data-driven approach to risk based decision making.
FAIR Institute member Darren Shady is an independent contractor and professional educator specializing cyber risk & FAIR’s data-driven approach to risk based decision making.
This article will explore how a shift towards quantitative risk analysis, particularly through the lens of the FAIR framework, can empower healthcare organizations to not only meet compliance requirements but also proactively manage risk, optimize resources, and make informed decisions.
With readily available frameworks and control libraries, essential knowledge is at our fingertips. The planned updates to the HIPAA Security Rule require written assessments of cyber threats, vulnerabilities, assets and risks. It’s a welcome step, and each proposed change is a necessary move to bring the industry in line with other sectors. However, these changes won't be easy or instantaneous. Organizations will need to re-prioritize and refocus, all while continuing to deliver quality patient care.
Healthcare organizations are already conducting risk analyses—whether for HIPAA compliance, HITRUST certification, or MIPS reporting. The annual security risk analysis required under MIPS is a prime example of risk assessment in practice. Instead of constantly reinventing the wheel, we should view the annual risk management plan as a natural outgrowth of continuous risk monitoring. Organizations are already collecting valuable security and compliance data—why not extract maximum value from it?
This shift is about more than just checking boxes for compliance; it provides tangible leverage. It strengthens our position when negotiating cyber insurance coverage, helps us determine which security investments truly reduce risk, and equips us with quantifiable risk data to confidently present to the board. The ability to demonstrate a structured, quantitative risk assessment significantly strengthens our case for favorable coverage terms and strategic resource allocation.
The Limitations of Traditional Risk Analysis (and Why FAIR Is Different)
Risk analysis must be approached as a top-down effort, aligning organizational priorities with key business risks. A structured, quantitative approach ensures that healthcare organizations focus on the most critical risks, rather than simply reacting to isolated threats.
One effective way to frame risk analysis is by focusing on "top risks"—the high-impact, high-likelihood loss events that could cause the most disruption. By examining these risks holistically, organizations can prioritize security investments based on actual business exposure, not theoretical concerns.
This contrasts sharply with the "boil the ocean" approach that many organizations adopt year after year. Producing voluminous data often creates a false sense of security. We should know our risks, especially after years of conducting risk assessments. Unfortunately, these assessments are often treated as snapshots in time, requiring a complete re-performance each year. We need to own our risks. Ask yourself, "What keeps me up at night?" and start there.
This realization can be a watershed moment. The old way of thinking defaults to a grassroots approach, attempting to solve control gaps and perceived threats from the bottom up. This inevitably leads to thousands of findings, with the best-case scenario being the identification of some commonality between controls or vulnerabilities, which are then framed as risks.
Traditional risk management—with its qualitative heat maps, ordinal scales, and subjective expert opinions—lacks the necessary defensibility and clarity. I recall reviewing a NIST-based assessment that generated thousands of scenario permutations. It was immediately clear that there was no way to present such an incoherent and overly complex report to the board. It lacked cohesion, actionable insights, and executive-level usefulness.
Without a structured framework like FAIR, risk management often devolves into addressing perceived control deficiencies without truly understanding the root causes. Is that true risk management, or simply reacting to symptoms?
Organizations transitioning from qualitative to quantitative risk analysis often begin by leveraging existing data sources, control frameworks, and incident records to establish measurable baselines. For example, a healthcare provider relying on compliance-based checklists might adopt FAIR’s structured loss event analysis to quantify the financial impact of ransomware on patient data availability. By shifting from generic risk categories to probabilistic modeling, leadership can better prioritize investments in controls that meaningfully reduce risk exposure.
Consider another scenario: a hospital network expanding its cloud-based patient records. Traditional risk assessments might classify cloud security as "moderate risk" and recommend vague mitigation strategies. A FAIR-based approach, however, would model the likelihood of data exfiltration, regulatory fines, and downtime costs, leading to smarter resource allocation—perhaps investing in insider threat monitoring rather than simply adding more endpoint protection.
Understanding FAIR: A Framework for Quantitative Risk Analysis
The FAIR Framework is not just another check-the-box exercise. It’s a set of quantitative risk models that enhances traditional risk management approaches and integrates seamlessly with existing frameworks like NIST CSF and CIS Controls. By combining FAIR with these frameworks, organizations can transition from compliance-driven security to data-driven, financially quantifiable risk management.
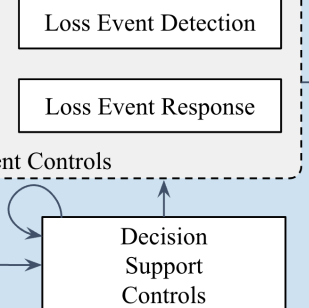
FAIR provides a hierarchical map defining the components of risk and their interrelationships. While additional sublayers exist for those seeking greater granularity, they aren't always necessary. FAIR's flexibility allows organizations to delve deeper when needed for complex analyses.
Integrated models make up the FAIR Framework
FAIR decomposes risk into measurable factors like Loss Event Frequency (LEF), Loss Magnitude (LM), Threat Capability, and Resistance Strength. The outputs aren't arbitrary scores, but tangible financial estimates that executives can act on. Instead of producing overwhelming amounts of data, FAIR distills risk into actionable insights.
Applying FAIR to a Real-World Healthcare Risk Event (Ransomware Example)
Let's illustrate with a realistic risk event: Ransomware Compromises a Regional Hospital System.
>>Threat Actor: A cybercriminal group leveraging a phishing campaign.
>>Threat Action: Employees unknowingly download a malicious attachment, triggering ransomware execution.
>>Asset at Risk: Electronic Health Records (EHR) and critical hospital infrastructure.
>>Vulnerability: Lack of multi-factor authentication (MFA) on remote access portals.
>>Predisposing Conditions: Limited staff security awareness training and outdated endpoint protection software.
>>Loss Magnitude: Disruption of patient care, regulatory penalties, reputational damage, and financial loss due to recovery costs.
Now, let's apply the FAIR model:
|
FAIR Risk Analysis: Ransomware Impact on a Hospital System |
|
|
FAIR Component |
Analysis |
|
Asset at Risk |
Electronic Health Records (EHR), patient monitoring systems, scheduling systems, and hospital infrastructure (e.g., imaging, pharmacy, labs). |
|
Threat Agent |
Cybercriminals deploying ransomware via phishing, exploiting unpatched vulnerabilities, or credential theft. |
|
Threat Event Frequency (TEF) |
Estimated based on hospital industry cyberattack trends and internal threat intelligence. Likely ranges between 1 to 5 times per year based on threat actor intent and capabilities. |
|
Contact Frequency (CF) |
Multiple vectors exist (email phishing, remote desktop exposure, supply chain software vulnerabilities), making contact frequency relatively high (daily to weekly). |
|
Probability of Action (PoA) |
Cybercriminals are financially motivated, and hospital systems represent high-value targets. Estimated PoA: 70%-90% per engagement. |
|
Susceptibility (Susc) |
Based on Threat Capability (TCap) vs. Resistance Strength (RS): Given known vulnerabilities in healthcare IT systems and limited segmentation, susceptibility is estimated between 50%-80% per event. |
|
Loss Event Frequency (LEF) |
TEF x Susceptibility, resulting in an estimated 1 ransomware event per 2-3 years. |
|
Primary Loss Magnitude (PLM) |
- Productivity Loss: Hospital downtime of 24-72 hours can disrupt thousands of patient visits and surgeries. |
|
- Response Costs: Incident response, forensic investigation, and system restoration estimated at $500K to $5M. |
|
|
- Replacement Costs: New security measures and hardware refreshes could cost $1M to $10M. |
|
|
Secondary Loss Event Frequency (SLEF) |
Given regulatory scrutiny (HIPAA), lawsuits, fines, and reputational fallout are probable in 40%-60% of cases. |
|
Secondary Loss Magnitude (SLM) |
- Fines & Judgments: Regulatory fines range from $100K to $5M, lawsuits can reach $10M+. |
|
- Reputation Damage: Loss of patient trust, potential long-term revenue impact of 5%-10% decline in patient volumes. |
|
|
- Competitive Advantage Loss: Potential decrease in insurer contracts and referrals due to trust erosion. |
|
|
Overall Risk Exposure |
Estimated $10M to $50M per event (Monte Carlo-based analysis would refine this further). |
|
FAIR-CAM based Control Recommendations |
- Avoidance Controls: Network segmentation, air-gapped backups, Zero Trust. |
|
- Deterrence Controls: Employee training, proactive threat intelligence. |
|
|
- Resistance Controls: MFA, EDR/XDR, immutable backups. |
|
|
- Detection Controls: SIEM with behavioral analytics, 24/7 SOC monitoring. |
|
|
- Response Controls: DR/BCP tabletop exercises, ransomware-specific IR playbooks. |
Conclusion: The Future of Quantitative Risk Management
Risk management isn’t about fear, uncertainty, and doubt—it’s about clarity, quantification, and strategic decision-making. By leveraging FAIR, organizations can move beyond compliance-driven exercises and turn risk management into a true business enabler.
Key Takeaways:
>>Improved Decision-Making: FAIR provides a structured, quantifiable approach that aligns risk management with financial and operational priorities.>>Better Resource Allocation: Quantitative risk analysis helps prioritize investments with the highest risk reduction.
>>Enhanced Regulatory Compliance: Organizations can exceed compliance requirements by demonstrating defensible risk assessments.
>>Stronger Cyber Resilience: A data-driven strategy ensures proactive responses to evolving threats.
The future isn’t about producing more scores—it’s about making better decisions.
Related Post: Accounting Authority ACCA Points to FAIR Standards for Healthcare Cyber Risk Management
Expect advances in quantitative cyber risk management coming from the FAIR Institute’s Health Industry Research Board. Are you a healthcare professional interested in participating? Contact us today.